Sustainable HAI Reductions Depend on Compliance Verification
Caregiver handwashing rates appear quite high right now, thanks to the COVID-19 scare. Fear is apparently a good driver but a likely temporary one. It is expected that these “COVID-19” handwashing rates will soon be returning to the pre-pandemic normal of 30-40%.
Today’s special situation is a unique window for operators to develop a handwashing program to institutionalize a new more patient-protective norm. Caregivers are likely at or close to where they should have been for years. Now all they have to do is maintain the new “status quo.”
The “new” handwashing must be risk-based but go beyond fear as the primary motivator. A process commensurate with the risk is required. It must be a measurable protocol and compliance data must exceed that gathered by secret shopper methods.
Caregiver engagement is best sustained by individual performance monitoring with data served up in a readily available reporting system where the caregiver is the first person to see his or her accountability “report card” and immediately take the self-corrective actions required.
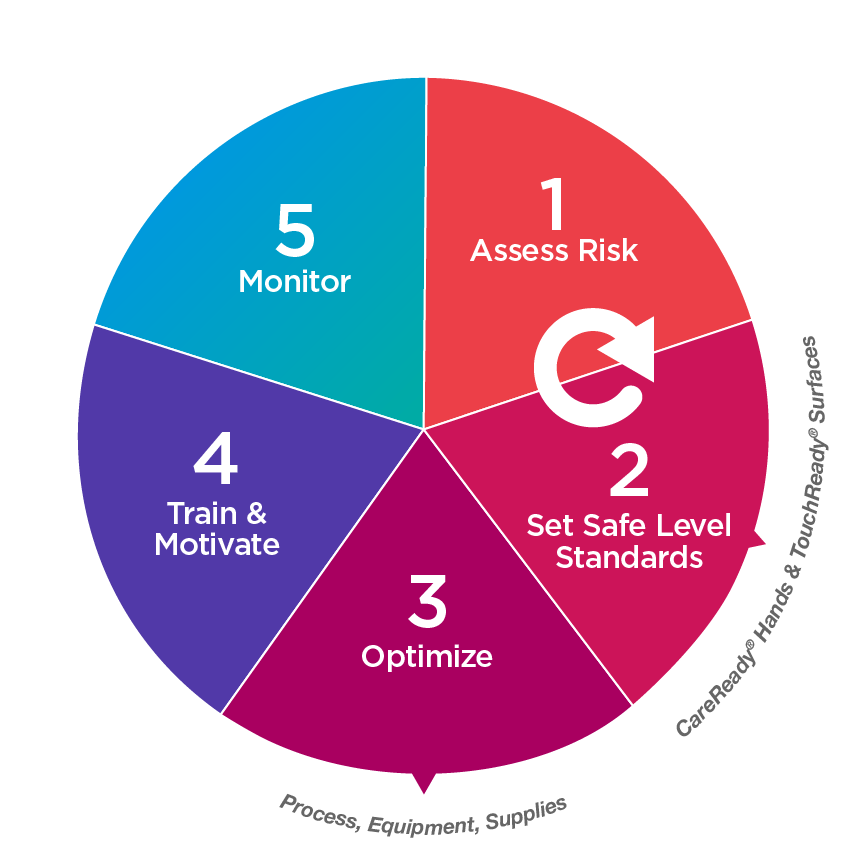
The institutionalizing process for a new program starts with an assessment of the risk and moves through 5 steps:
Step 1 is critical as it will define the process and the budget. A poorly conducted Risk Assessment is the common source of excuses for the 30% compliance. “No time” is no excuse.
RiskNomics is an important resource available to help establish the risk parameters while dealing with the budgetary realities.
This Step 5, Monitor & Verify, example summarizes the case for electronically assisted handwash performance monitoring. More handwashing saves lives.
“Breaking the Chain of Transmission: Addressing the 3 Most Common Sources of HAIs” is a webinar presented by Dr. Hudson Garrett Jr. It provides a solid foundational review of handwashing and more.


