Sixteen years of formal and informal research has provided the Handwashing For Life Institute with a long list of reasons and excuses for low handwashing rates. Today caregivers may hear of their compliance rate being reported at 90% but in their heart of hearts know it is far short of the reported number. Now with the Joint Commission focusing on continuous improvement as their auditing standard for handwashing, hospitals and nursing homes may want to reassess the why for their rates being less than satisfactory.
The long list of causes has been distilled into five all-inclusive categories. This Handwashing Hurdles graphic is used as a tool of collaboration to gather multi-department views, exploring this question “Which of these applies to our operation, our unit?”
Consider this exercise with a large or small group. Prioritize the five factors by printing the attached graphic as a 24″ x 36″ chart. Give particpants three different colored dots, indicating their rank.
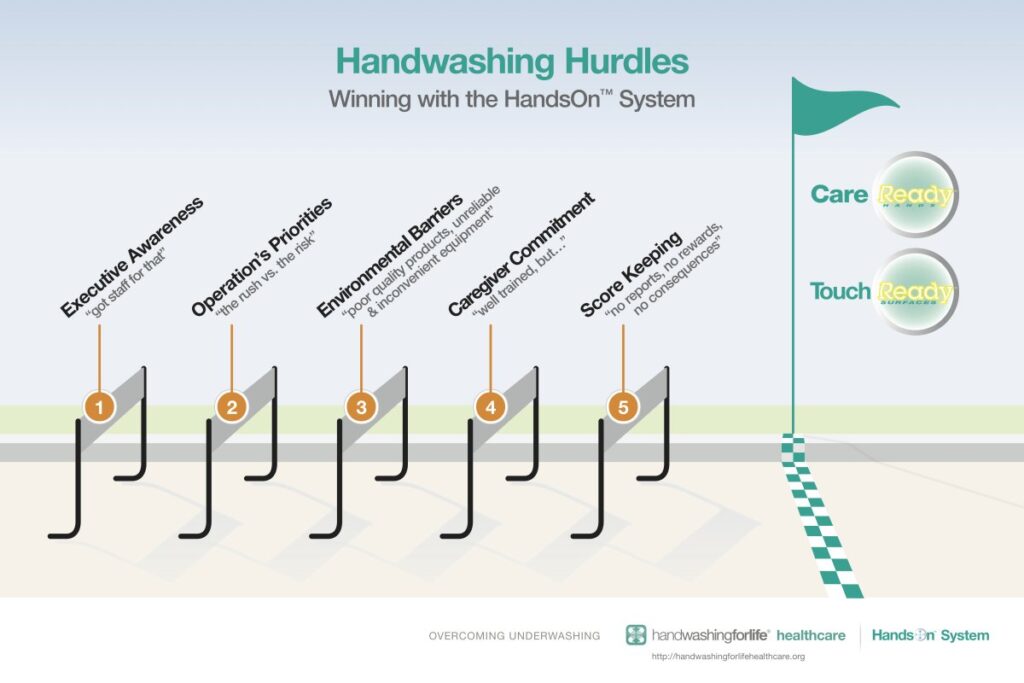
Hurdle 1: Executive Awareness “got staff for that”
Is it a matter of awareness or complacency? Have we unwittingly shifted our good record regarding outbreaks into our healthcare culture giving us an unwritten reason for accepting risky hand hygiene practices? Knowing that we have a good legal team behind us, are we not challenging low compliance rates? Consider conducting a Handwashing For Life Hand Hygiene Audit, starting with the 5 Hurdles exercise.
Hurdle 2: Operation’s Priorities “the rush vs. the risk”
Frequent handwashing competes with productivity for staff time. Increased regulations and more demands on caregivers for matters other than dealing directly with the patients take their toll. Both the manager and each member of the staff need agreed standards for both the quality and frequency of handwashing.
Hurdle 3: Environmental Barriers “poor quality products, unreliable and inconvenient equipment”
Poor location of dispensers, user-unfriendly supplies and unreliable equipment deter frequent and timely handwashes. Install time-saving, health protecting electronic faucets and touch-free dispensers. If the soap is not task-formulated and damages skin, frequent washing is unlikely. Paper toweling that disintegrates on wet hands is another deterrent to frequent soap-water handwashing. Better soaps and paper towels pay dividends in compliance and risk reduction.
Hurdle 4: Caregiver Commitment “well trained, but . . . “
When caregivers don’t want to wash, they won’t. They are more influenced by example than training. Check hiring policies to see if the core qualities needed for patient safety are being specified. Then turn to training with plenty of personalization and visualization remembering that there is a training ceiling. Training alone does not normally deliver sustainable gains. Employee turnover taxes training resources and is one of the more common excuses for poor handwashing compliance. Establish turnover norms to assure healthcare standards are met within the context of continuous improvement.
Hurdle 5: Score Keeping “no reports, no rewards, no consequences”
Even good managers have limits to their span of leadership. Control is best enhanced by motivating staff with data that measures positive behaviors. Consider adding compliance monitoring technology to document and reward the winners. Data helps sustain improved handwashing behaviors.


