Facing the culture trap
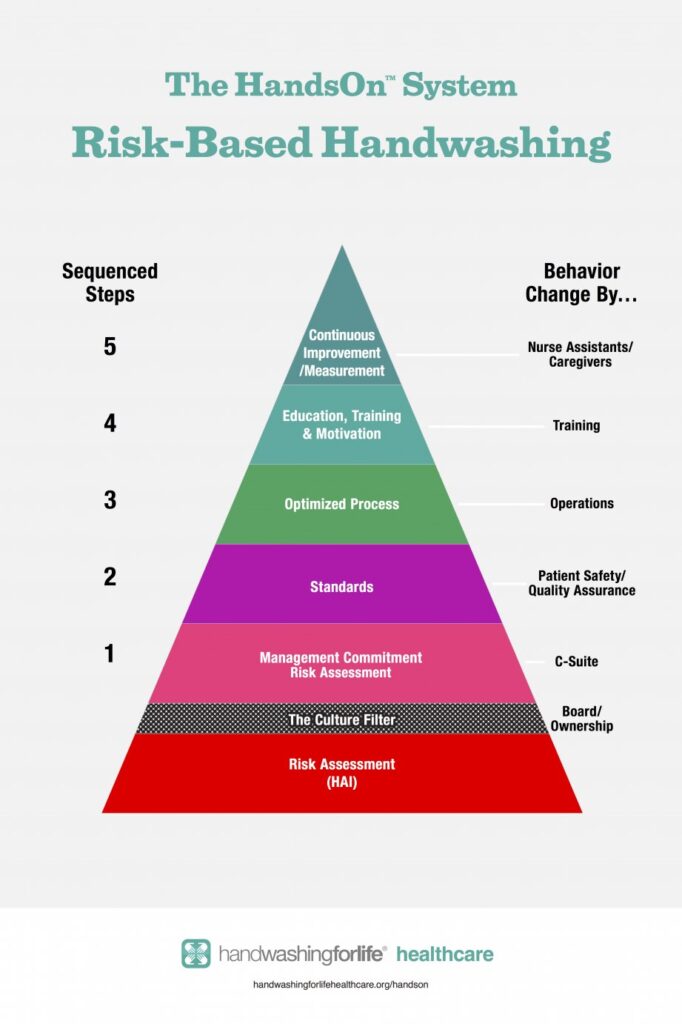
Handwashing behaviors are primarily driven by an assessment of risk. The Administration starts near the top of this pyramid, looking first to change the behaviors of caregivers via Nursing, Quality Assurance and Training. The C-Suite representatives are disengaged as there are no handwashing compliance reports to look at. They are content that Nursing & Operations has this under a modicum of control, undeterred by their inherent bias of productivity.
Technology savvy members of the facility focus on the severity factor of potential outbreak driven legal actions while the C-Suite looks more at probability, weighted heavily by personal experience. This disconnect has defined the predominant healthcare culture for decades, one based on subjective departmental interpretations without integrated metrics. This unwritten “policy” maintains the status quo, organizational peace and job security. It serves as an informal compass for decision making where reassurance is nurtured by two presumed realities: “Productivity and profits come first” and We have not recently had an outbreak.”
Technical risks are commonly defined clearly by Infection Prevention and Quality Assurance but, without handwash standards, their assessment lies dormant and disengaged from the network of corporate reporting – at least until an outbreak exposes system failure.
The solution to protect the healthcare facility with enhanced handwashing makes sense at every level but multi-department collaboration on this topic rarely includes C-Suite representatives. The real risk languishes in the base of this solution pyramid, filtered out by the current culture.
What does this mean to a facility’s goal of patient care and continuous improvement? Perhaps no one really wants to know as documented knowledge would force change at every level. It could open Pandora’s box and expose firms to unforeseen legal actions. Technology is threatening today’s practices of complacency and inadvertant concealment. There are new methods to search more and find those weak links in the chain of patient and resident protection. Whole Genome Sequencing, WGS, leads the traceability advances.
Actual tracking of handwashing has been greatly facilitated by wireless data collection. Prices on these technologies have plummeted, making it affordable for even smaller independent healthcare facilities.
There is a growing legal threat to accompany that of Strict Liability and that is the choice not to use readily available hand hygiene technologies. In the coming years we may see this applied to outbreaks where the lack of handwashing is a contributing factor. This principle has been dubbed by Handwashing For Life as the “Ignored Intervention.” This could be a multiplier in plaintiff awards and add to the Department Of Justice’s increasing threat of executive jail time.
The HandsOn™ process can sustainably change handwashing behaviors at all levels once data is available to drive continuous improvement. The early adopters of handwash monitoring systems, those that step forward now and invest in this new technology, are true leaders. In the end, the tracking of handwashing becomes a mirror of their mission statement, culture and a predictor of innovation, growth and longterm viability.


